A hiatal hernia occurs when the upper part of your stomach bulges through the diaphragm into the chest cavity. This common condition affects up to 60% of people over age 50 and can lead to acid reflux or GERD. At Malladi Bariatrics & Advanced Surgery in Dallas and Plano, we specialize in diagnosing and treating hiatal hernias with minimally invasive techniques. This updated 2025 guide covers symptoms, causes, treatments, and more to help you understand and manage this condition.
What is a Hiatal Hernia?
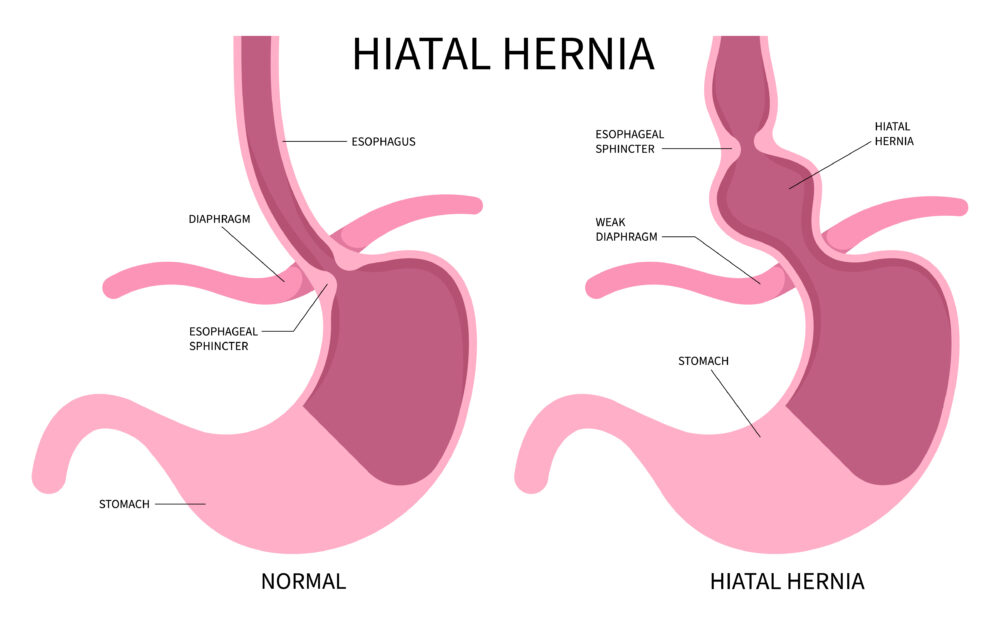
The diaphragm is a muscle that separates the chest from the abdomen, with a small opening called the hiatus for the esophagus to pass through. In a hiatal hernia, the stomach pushes up through this hiatus. There are two main types:
- Sliding Hiatal Hernia (Type I): The most common (95% of cases), where the stomach and esophagus slide into the chest.
- Paraesophageal Hiatal Hernia (Types II-IV): Rarer, where part of the stomach squeezes beside the esophagus, potentially causing complications.
Small hernias often go unnoticed, but larger ones may require treatment. If you’re in Dallas and experiencing related issues, contact Dr. Malladi for a consultation.
Hiatal Hernia Symptoms
Many hiatal hernias are asymptomatic, but when symptoms occur, they often mimic GERD or acid reflux. Common signs include:
- Heartburn, especially after eating or lying down.
- Regurgitation of food or sour liquid into the mouth.
- Chest pain or discomfort (non-cardiac).
- Difficulty swallowing (dysphagia).
- Belching, bloating, or indigestion.
- Shortness of breath or fatigue.
- Vomiting blood or black stools (indicating bleeding).
If you notice these symptoms, seek evaluation from a reflux surgeon like Dr. Malladi in Dallas to rule out complications.
Causes of Hiatal Hernia
The exact cause isn’t always clear, but weakened diaphragm muscles allow the stomach to protrude. Contributing factors include:
- Age-related changes (most common in people over 50).
- Increased abdominal pressure from coughing, vomiting, straining, or heavy lifting.
- Obesity, which adds strain to the diaphragm.
- Smoking, which weakens tissues.
- Injury or trauma to the area.
- Congenital defects, such as a larger-than-normal hiatus.
Risk factors like pregnancy or chronic conditions (e.g., COPD) can also play a role. Maintaining a healthy weight through bariatric services may reduce your risk.
Diagnosis of Hiatal Hernia
Hiatal hernias are often found incidentally during tests for acid reflux. Diagnostic methods include:
- Upper Endoscopy: A camera examines the esophagus and stomach for inflammation.
- Barium Swallow X-ray: You drink a contrast liquid to highlight the hernia on imaging.
- Esophageal Manometry: Measures swallowing muscle coordination.
- pH Monitoring: Assesses acid reflux levels.
Dr. Malladi in Dallas uses advanced diagnostics to confirm hiatal hernias and plan personalized treatment.
Complications of Hiatal Hernia
Untreated hiatal hernias can lead to:
- Chronic GERD or acid reflux.
- Esophagitis (inflammation of the esophagus).
- Barrett’s esophagus (precancerous changes).
- Strangulation or obstruction (rare, but an emergency in paraesophageal types).
- Bleeding or ulcers.
Early intervention prevents these issues. If you’re experiencing complications, explore hiatal hernia repair.
Hiatal Hernia Treatment Options
Treatment depends on symptoms and hernia size. Options include:
Lifestyle Remedies and Prevention
- Eat smaller, frequent meals and avoid lying down after eating.
- Avoid trigger foods like fatty, spicy, or acidic items (e.g., chocolate, caffeine, onions).
- Maintain a healthy weight and quit smoking.
- Elevate the head of your bed by 6-8 inches.
- Manage stress and avoid heavy lifting.
These changes can prevent worsening and reduce acid reflux.
Medications
- Antacids (e.g., Tums) for quick relief.
- H2-receptor blockers (e.g., famotidine) to reduce acid production.
- Proton pump inhibitors (PPIs like omeprazole) for stronger control and healing.
Surgery
For severe cases or when meds fail, laparoscopic hiatal hernia repair is effective (90% success rate). Dr. Malladi performs minimally invasive surgery in Dallas, pulling the stomach back, tightening the hiatus, and often adding fundoplication to prevent reflux. This outpatient procedure uses small incisions for faster recovery.
Why Choose Dr. Malladi for Hiatal Hernia Treatment in Dallas?
Dr. Preeti Malladi, a board-certified bariatric surgeon, has extensive experience in hiatal hernia repair and reflux surgery. Serving Dallas and Plano, she offers personalized care with advanced laparoscopic techniques. Schedule a consultation to discuss your options.
Frequently Asked Questions
What are the main symptoms of a hiatal hernia?
Common symptoms include heartburn, chest pain, regurgitation, and difficulty swallowing. See our GERD guide for more.
What causes a hiatal hernia?
Causes include age, obesity, smoking, and abdominal pressure. Lifestyle changes can help prevent it.
When is surgery needed for hiatal hernia?
Surgery is recommended for severe symptoms or complications unresponsive to meds. Dr. Malladi specializes in laparoscopic repair in Dallas.
Can hiatal hernia be prevented?
Yes, by maintaining a healthy weight, avoiding triggers, and quitting smoking. Explore obesity management options.
How long is recovery from hiatal hernia surgery?
Most patients recover in 1-2 weeks with laparoscopic methods. Contact us for details.
Contact Dr. Malladi for Hiatal Hernia Care in Dallas
If you suspect a hiatal hernia or need treatment in Dallas or Plano, contact us today!
